Third Symposium on Cancer in Latino Communities highlights education as the key in the fight against cancer
Philadelphia, PA — Early cancer screening saves lives: education is key and makes the difference. That was the central message of the Third Annual Symposium on Cancer in Latino Communities (including Latino/Hispanic and Latinx populations), organized by the Society of Ibero and Latin American Medical Professionals (SILAMP), the National Hispanic Medical Association (NHMA), the Latino Medical Student Association (LMSA), and the Sidney Kimmel Cancer Center (SKCC).
This academic event, focused on the diagnosis and treatment of cancer in Hispanic patients, took place on November 1 at Thomas Jefferson University in Philadelphia.
The symposium brought together specialists, students, and members from various health disciplines to address the unique challenges Latinos face in cancer diagnosis and treatment, from cultural and linguistic differences to socioeconomic and immigration-related barriers.
“We want future health professionals to understand the needs of Latino patients better and to provide more inclusive, respectful, and effective care,” said Clara Granda–Cameron, DrNP, associate professor at the Jefferson College of Nursing in Philadelphia and moderator of the mentorship panel.

DATA UPDATES
Among the data presented, Dr. Cherie P. Erkmen, MD, professor of thoracic surgery at Temple University’s Lewis Katz School of Medicine, noted that “lung cancer causes more deaths (342 per day) than breast, prostate, and colorectal cancers combined.” She indicated that lung cancer remains the leading cause of cancer death globally, followed by breast cancer in second place.
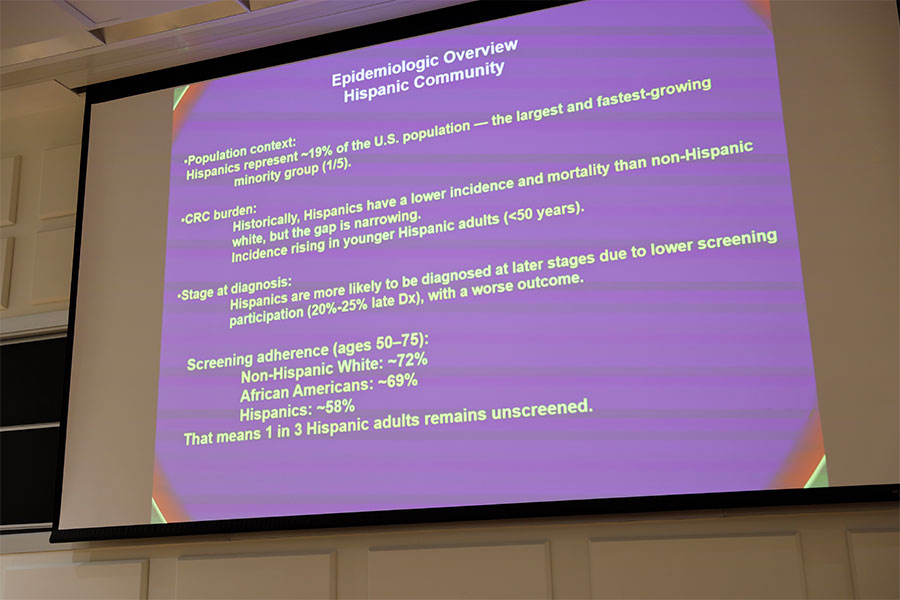
Colorectal cancer, meanwhile, is the third most common cancer and the fourth leading cause of cancer deaths worldwide, according to Dr. Ricardo Morgenstern, MD, clinical associate professor in the Division of Gastroenterology–Hepatology at the Perelman School of Medicine, University of Pennsylvania.
POTENTIAL RISKS
Dr. Curtis Miyamoto, MD, professor of radiation oncology and associate director of Clinical Services at the Fox Chase Cancer Center at Temple University Hospital, spoke about the potential risks faced by janitors, nurses, cashiers, custodians, and caregivers—jobs often held by immigrants—who may be exposed to harmful chemicals such as cleaning agents and pesticides. He emphasized the link between this exposure and the potential development of breast cancer.
To reduce that risk, it is essential to first identify these hazards, then provide multilingual education and training to promote safe workplace practices, and develop health policies that protect vulnerable immigrant workers.
Dr. Miyamoto also drew attention to recent American Cancer Society (ACS) statistics regarding Invasive Lobular Carcinoma (ILC), a type of breast cancer that is difficult to detect early and has been increasing more sharply than other forms. It is estimated that 33,600 women in the U.S. will be diagnosed with ILC in 2025.
Ana María López, MD, MPH, MACP, event organizer, is a professor and vice chair of the Department of Medical Oncology at Sidney Kimmel Medical College, and director of the New Jersey Division of the Sidney Kimmel Cancer Center at Thomas Jefferson University.
RESOURCES FOR HISPANICS
One of the panels featured members from Puentes de Salud, including Dr. Daphne Owen, MD, Director of Medical Education, and José Ortiz, Clinical Research Coordinator, as well as Carlos Obrador, Consul of Mexico in Philadelphia. They all highlighted the efforts their organizations are making through public awareness campaigns, early detection testing, and strategic partnerships for treatment and follow-up.

Consul Obrador emphasized the “Ventanillas de Salud” (Health Windows) program at his consulate, which provides access to healthcare services for people who otherwise could not obtain them. He noted that, “while access to other consular services is limited to Mexican nationals, the Mexican Consulate’s health programs are open to everyone, regardless of nationality.”
Dr. Ana María López, professor of Medical and Integrative Oncology and Nutritional Sciences at Thomas Jefferson University, stressed the importance of nutrition, not only as a preventive factor against cancer but also as an ally during and after treatment. She explained that what we eat “can cause inflammation,” and advised:
“Eat as many plants as possible; choose them for breakfast, lunch, snacks, and dinner; always include vegetables.”
Then, She added: “When a healthy person has inflammation, a diet rich in fruits and vegetables can reduce it. But during cancer treatment, fresh fruits and vegetables can be harder to digest; so, soups with well-cooked vegetables may be better. The body is more delicate during treatment, but later, it’s important to return to eating foods that cause less inflammation.”
Regarding breast cancer statistics among Latinas, Dr. López noted: “While overall breast cancer incidence among Latina women in the U.S. is lower, we know that the Latino population here is younger, so cases tend to occur among younger women.”

Her advice: “Talk to your doctor and get screened; early detection saves lives.”
This was a message echoed by Dr. Cherie Erkmen, who added, “Don’t be afraid to know. We need to learn more; screening tests can lower your cancer risk, even with something as simple as a chest X-ray or CT scan every year for those at high risk of lung cancer.”
Among Latinos, however, fear of a cancer diagnosis often leads many to refuse early screenings, choosing instead to “leave it in God’s hands.”
Another serious challenge is that many Latinos lack health insurance (26% vs. 9% among non-Hispanic whites). Limited information about which tests to take and when also leads to late diagnoses, and there is a higher prevalence of cancers such as cervical (HPV-related) and stomach cancer (H. pylori-related).

When it comes to health, as in all things, information is power.
And you—what are you doing to prevent cancer?